Home Health Comfort Care Documentation Best Practices

Home Health Comfort Care Documentation Best Practices
As a home health care provider, accurate and thorough documentation is crucial to ensure that patients receive high-quality care and that your agency remains compliant with regulatory requirements. Comfort care, also known as palliative care or hospice care, presents unique documentation challenges due to its focus on alleviating symptoms and improving quality of life rather than curing illnesses. In this article, we will outline best practices for documenting comfort care services in home health settings.
Importance of Accurate Documentation

Accurate and complete documentation is essential for several reasons:
- Reimbursement: Accurate documentation helps ensure that your agency receives proper reimbursement for services rendered.
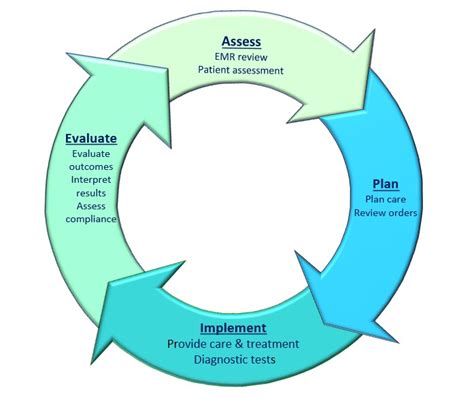
- Quality of care: Thorough documentation enables healthcare providers to track patient progress, identify areas for improvement, and adjust care plans as needed.
- Regulatory compliance: Home health care agencies must comply with various regulations, including those related to documentation. Accurate documentation helps agencies demonstrate compliance and avoid penalties.
- Patient safety: Incomplete or inaccurate documentation can compromise patient safety by leading to misunderstandings or miscommunications among healthcare providers.
Key Elements of Comfort Care Documentation

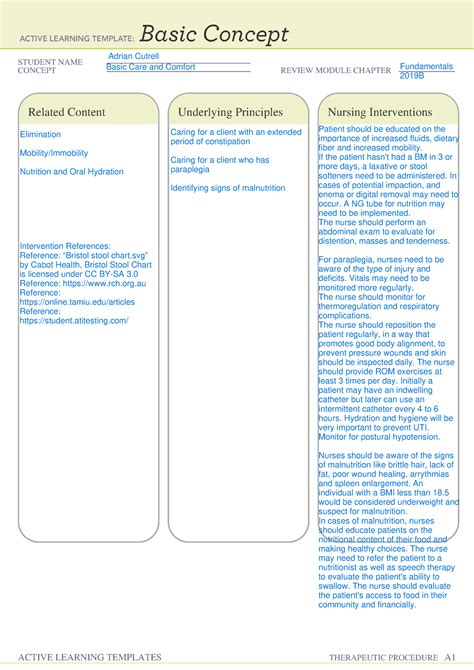
To ensure that your documentation meets best practices, focus on capturing the following key elements:
- Patient goals and preferences: Document the patient’s goals, values, and preferences regarding their care, including any advance directives or living wills.
- Care plan: Develop and document a comprehensive care plan that outlines the patient’s specific needs, interventions, and expected outcomes.
- Symptom management: Document the patient’s symptoms, including their severity, frequency, and impact on daily life, as well as the effectiveness of interventions aimed at managing those symptoms.
- Medication management: Document all medications, including dosages, frequencies, and any changes or adjustments.
- Collaboration and communication: Document communication with other healthcare providers, family members, and caregivers, including any changes to the care plan or concerns raised by these stakeholders.
- Progress and outcomes: Regularly document the patient’s progress and outcomes, including any changes in condition, symptoms, or functional status.
Best Practices for Documenting Comfort Care Services
To ensure that your documentation meets best practices, follow these guidelines:
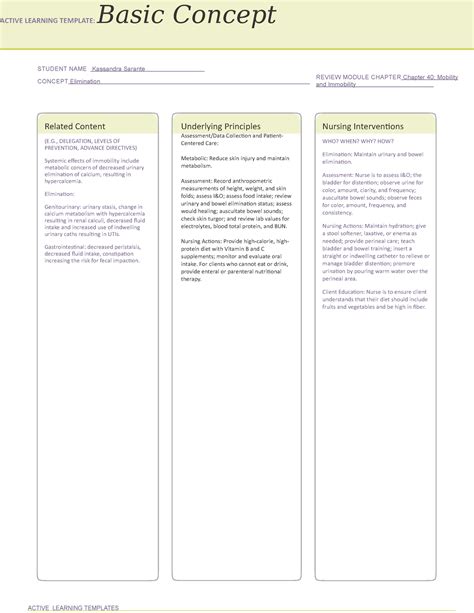
- Use a standardized format: Use a standardized documentation format to ensure consistency and ease of use.
- Be thorough and detailed: Document all relevant information, including patient goals, care plans, symptom management, medication management, and progress.
- Use clear and concise language: Avoid using jargon or technical terms that may be unfamiliar to non-clinical staff or family members.
- Document in real-time: Document patient information in real-time, rather than relying on memory or delayed documentation.
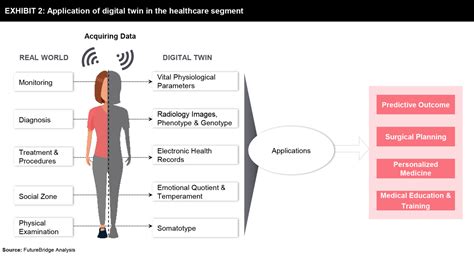
- Use electronic health records (EHRs): Consider using EHRs to streamline documentation, improve accessibility, and reduce errors.
| Documentation Element | Best Practice |
|---|---|
| Patient goals and preferences | Document patient goals and preferences clearly and concisely, using the patient's own words whenever possible. |
| Care plan | Develop and document a comprehensive care plan that outlines the patient's specific needs, interventions, and expected outcomes. |
| Symptom management | Document the patient's symptoms, including their severity, frequency, and impact on daily life, as well as the effectiveness of interventions aimed at managing those symptoms. |
📝 Note: Use a standardized format for documenting patient information to ensure consistency and ease of use.
Challenges and Solutions in Comfort Care Documentation

Comfort care documentation presents unique challenges, including:
- Capturing subjective data: Comfort care focuses on alleviating symptoms and improving quality of life, which can be subjective and difficult to quantify.
- Managing complex medical regimens: Comfort care patients often have complex medical regimens, including multiple medications and therapies.
- Collaborating with multiple stakeholders: Comfort care involves collaboration with multiple stakeholders, including family members, caregivers, and other healthcare providers.
To overcome these challenges, consider the following solutions:
- Use standardized assessment tools: Use standardized assessment tools, such as the Palliative Performance Scale (PPS) or the Edmonton Symptom Assessment System (ESAS), to capture subjective data.
- Develop a medication management plan: Develop a comprehensive medication management plan to ensure that medications are properly managed and documented.
- Use communication templates: Use communication templates to facilitate collaboration and communication with multiple stakeholders.
💡 Note: Use standardized assessment tools to capture subjective data and develop a comprehensive medication management plan to ensure proper management and documentation of medications.
Home health comfort care documentation requires attention to detail, accuracy, and completeness. By following best practices and using standardized formats, you can ensure that your documentation meets regulatory requirements and supports high-quality patient care.
FAQ Section:
What is the importance of accurate documentation in home health comfort care?

+
Accurate documentation is essential for ensuring that patients receive high-quality care, and that your agency remains compliant with regulatory requirements. It also helps ensure proper reimbursement for services rendered.
What are the key elements of comfort care documentation?
+
The key elements of comfort care documentation include patient goals and preferences, care plan, symptom management, medication management, collaboration and communication, and progress and outcomes.
What are some best practices for documenting comfort care services?
+
Best practices for documenting comfort care services include using a standardized format, being thorough and detailed, using clear and concise language, documenting in real-time, and using electronic health records (EHRs).